The Breast Cancer Research Foundation of Alabama (BCRFA) enthusiastically announces its continued dedication to support breast cancer research in Alabama through a significant investment of $1,125,000 in 2024.
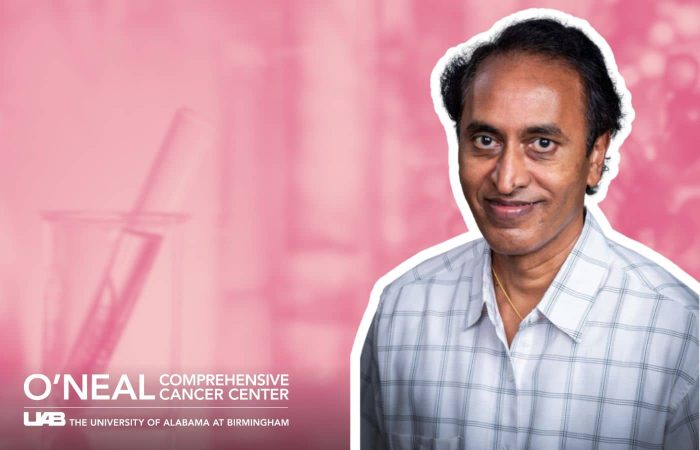
Leveraging BCRFA funds, UAB researcher lands $1.7M grant
Selvarangan Ponnazhagan, Ph.D. recently received a $1.7 million R01 grant from the National Cancer Institute for his study on breast cancer bone metastases (breast cancer that has spread to the bones). In recent years, the BCRFA provided grant support for the earlier stages of this work, allowing Ponnazhagan to collect the large amounts of preliminary data required to apply to national funders.
Ponnazhagan’s NCI research is titled “Mechanisms and Therapeutic Targeting of Osteoimmune Functions of RANKL in Breast Cancer.”
A release from UAB’s Department of Pathology at the Heersink School of Medicine gives more detail on the project:
Current treatments for patients with breast cancer bone metastases have shown that targeting tumor cells alone is not sufficient for long-term survival, but a multi-faceted approach is needed to inhibit tumor cells in the bone microenvironment that drive immunosuppression and tumor growth. As breast cancer spreads throughout the bone, tumor cells interact with infiltrating immune cells and reactive stroma in the microenvironment. This results in the production of cytokines and other soluble proteins necessary for cell signaling that activate the expression of nuclear factor kappa-B ligand (RANKL) leading to aggressive bone damage.
“We want to expand our understanding of the roles of RANKL in immune suppression and bone damage,” Ponnazhagan says. “We will test the potential of a combination therapy to reverse tumor-associated pathology on immune and skeletal systems.”
The first part of the team’s study will elucidate the role and mechanisms of upregulated RANKL in tumor cells. Next, they will work toward developing a biologically-driven systemic therapy for pre-metastatic and metastatic breast cancer, targeting the protumorigenic osteoimmune functions of elevated RANKL.
“We’re proposing a genetically engineered cell therapy, expressing an osteoprotegerin (OPG) variant we developed by structure-based protein engineering,” Ponnazhagan says. “We found that its application in pre-metastatic disease significantly decreases metastasis of breast cancer in vivo.”
Ponnazhagan’s team will employ immunocompetent mouse models to determine the role of RANKL both in protumorigenic myeloid cell function and non-canonical signaling on programmed death-ligand-1 (PD-L1) expression during breast cancer bone metastasis and interpret the therapeutic effects of the OPG variant by additionally dampening PD-L1 levels. The OPG variant cell therapy will be tested further with a programmed cell death protein 1 antibody and chemotherapy in pre-metastatic and metastatic breast cancer.
“The knowledge from this study will assist in developing a biologically driven combination therapy that addresses immune suppression, tumor growth, and skeletal-related events to extend the life expectancy of patients, especially those with pre-metastatic high-risk breast cancer,” Ponnazhagan says.
“I am grateful for the support provided by the BCRFA through pilot funding that allowed us to generate preliminary data for a successful R01 grant from the NIH/NCI” concludes Dr. Ponnazhagan.